Neobladder
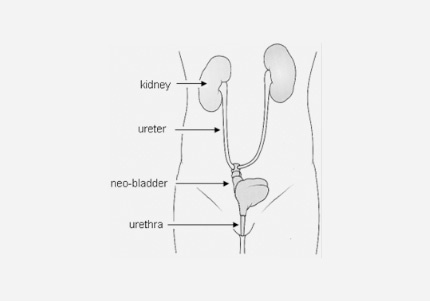
It may be possible, in the course of your radical cystectomy (bladder removal) for your surgeon to create an artificial bladder. A neo-bladder is a replacement bladder created from a section of your bowel and attached to your urethra, which means you can pass urine in the same way as with a normal bladder. It is known as an orthotopic neobladder (which means ‘same place' and ‘new bladder').
What happens during a bladder reconstruction
During radical cystectomy the whole bladder is removed but part of the urethra remains in place. In the case of neobladder surgery, the surgeon creates a replacement reservoir (neobladder) from a segment of bowel. The ureters (the tubes linking kidneys and bladder) are connected to the neobladder and this is then connected to the urethra. A catheter is put through the urethra into the new bladder and left for 2-4 weeks until the joints have healed. The catheter is then taken out.
Benefits of neobladder
Once fully functional, a neobladder means you can usually pass urine as with a normal bladder and it avoids the need for an external device to collect urine. This type of urinary diversion may allow patients to return to a routine as close to normal as possible.
Who is an orthotopic neobladder not suitable for?
Not all patients who have a cystectomy are suitable for this surgery. There must be no evidence of cancer in the surrounding tissue, patients must have good health and be committed to regular follow up to look after their neobladder after their surgery.
Reasons why patients may be unsuitable for a neobladder after radical cystectomy include:
- high risk tumours which are at risk of recurrence especially within the urethra which is left in place
- existing kidney dysfunction
- liver dysfunction
- bowel disease / dysfunction - (for example Crohn's disease)
- previous radiotherapy
- poor patient memory/mobility/manual dexterity
- non-compliant with follow up
- incontinence prior to their surgery
This list is not exhaustive and this should be discussed fully with your surgeon in your outpatient appointment prior to the surgery.
What to expect after surgery
After your surgery you should expect to have a number of tubes coming out of your abdomen, which will include a urinary catheter from your urethra. There may be other tubes coming out of the abdomen including another catheter coming out through the abdominal wall.
These catheters allow the neobladder to heal without overfilling and will let you flush your neobladder with sterile water regularly to remove mucus (the bowel lining normally produces mucus and without flushing this might block the catheter and stop the neobladder from draining). You will also have ureteric stents, which stay in place while the join between the ureters and the neobladder heals. The stents and catheters will be removed once your neobladder has healed. You may have X rays before the catheters are removed.
Passing Urine with the neobladder
After the catheters are removed you will be taught how to regularly empty your neobladder. After the operation, you will produce urine in the normal way which will drain into your new bladder where it will be stored until you empty it. You won't have the same sensation of a full bladder as it used to be when you had your original bladder. Some people with neobladders say that they have a feeling of fullness in the abdomen or it's a bit like having wind.
At first, your new bladder can hold less than a normal bladder, but this will gradually increase over time. You will need to empty your bladder every one to three hours at first. After about three to six months your neobladder should build to a capacity of about a pint of urine (similar to a normal bladder).
If you are unsure, it's a good idea to empty your bladder at regular intervals of three to four hours. You want to avoid the risk of overfilling when the bladder would not drain properly. Many people who have a neobladder need to relax their pelvis and contract abdominal muscles to create some pressure or strain to empty their new bladder.
At night it is recommended that you get up to empty your neobladder at least once or twice before it becomes full. Use an alarm clock to make sure you wake up. Many patients will experience leakage at night over the first couple of months. It can also happen when you cough, laugh or strain. Pads may be useful in the first weeks/months after surgery.
Pelvic floor exercises and bladder training can help tone the right muscles and leakage should gradually improve. Your hospital team will be able to talk to you about these exercises. Also, as the new bladder stretches it will be able to hold more, so you will not need to empty it as often.
You will be taught how to pass a catheter into your new bladder. This is because you may sometimes need to use a catheter to make sure you have fully emptied your bladder. You want to make sure you don't leave a large amount of urine behind in your bladder as it might cause infection, difficulty with leakage and kidney problems.
How often you need to do this will depends how often and how much urine you are passing. You will probably be asked to keep a diary of your urine output for the first couple of months to help work out what is best for you. It does not take most people long to learn to pass a catheter. As long as it is done under clean conditions it can be done easily almost anywhere. The catheters are free on prescription.
You do need to drink plenty of fluid to keep the neobladder flushed in the first instance. In addition you may be discharged on bicarbonate tablets. This is because the urine is acidic and may be absorbed by the new bladder into the blood stream. The bicarbonate (an alkali) will counteract this.
You will be followed up after your discharge with regular scans and blood tests.
Your Stoma Nurse may be able to put you in contact with other patients who have had the same operation to allow you to ask questions and prepare yourself for the surgery and post operative neobladder management. If there is a bladder cancer support group locally, this can also be a good way to meet others who have had this operation.
The Urostomy Association can also be a useful source of advice and ongoing support.
How we help you
Latest News / Events
Setting up a support group for your patients - Webinar for Nurses - Mon 18 Aug 2025 08/07/2025
This is a FREE ABC UK online Zoom session, which is being run in response to requests from urology and cancer nurses, on how to set up and run a successful patient support group. The session will be led by one of the ABC UK Patient Support team, together with two advanced nurse specialists...