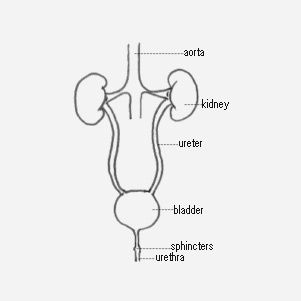
A Urostomy is one of the ways of creating this new route for the urine and for keeping your kidneys working efficiently.
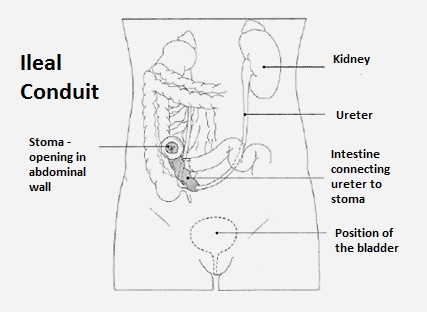
Your surgeon will attach the ureters to a segment of bowel to divert urine to the outside of the body through a stoma and into a pouch. This is called an ileal conduit diversion.
The conduit is made from a small detached section of the part of your bowel called the small intestine which is known as the ileum. The rest of the bowel is then joined up so your bowels continue to function normally. The ureters are attached to the segment of ileum, one end is closed up and the other open end is then brought through an opening in the abdominal wall to form a stoma. Stoma is Greek for mouth.
Narrow plastic tubes called stents will be inserted into the ureters from the kidneys to help keep urine flowing freely until things have healed. The stents are either taken out about 10 days after the surgery or they will come out by themselves.
Having a change in how you pass water will require some getting used to. A stoma nurse will usually see you before and after your surgery to advise on the best site for your urostomy and to support you in looking after the urostomy until you can do this independently.
After your surgery you will be managed according to a set protocol. Initially, after the surgery, you will see the ureteric stents (small plastic tubes) emerging from the urostomy. These stents allow the urine to bypass the area where the ureter joins the ileum until this anastomosis (the medical word for a surgical connection) has healed. These stents will be removed when your surgeon is happy that the join has fully healed. Urine is collected in a bag that is attached to the abdominal wall over the stoma. The bag can be emptied on a regular basis into the toilet and changed as advised by a stoma nurse.
The use of bowel for urinary diversion causes loss of essential salts in the urine. The levels of these salts will need to be monitored and dietary supplements may be required.
The stoma
A healthy stoma looks red. It is not painful to touch. As the conduit is made from a piece of bowel a blood supply is just under the surface so sometimes a little blood is seen when the stoma is cleaned. This is not unusual and can decrease over time. A white mucus might also be seen in the urine and on or around your stoma, again this is due to the lining of the bowel used, is quite normal and may also gradually decrease.
Your stoma nurse may be able to put you in contact with other patients who have had the operation to allow you to ask questions and prepare yourself for the surgery and post operative stoma management. If there is a bladder cancer support group locally, this can also be a good way to meet others who have had this operation.
ABC UK has helpful information sheets - you can find all our patient materials on our Resources page and you can download these or order print copies using our online order form or contact us directly.
Living with a Urostomy file LIVING WITH A UROSTOMY MAR 2019.pdf
Living with a Urostomy - tips from patients LIVING WITH A UROSTOMY PATIENT TIPS 2020.pdf
Urostomy bags
Urostomy bags are available on prescription to those who need them and there is a wide range of manufacturers and types of bag available. Your Stoma Nurse will provide advice as to which is most suitable for you to use.
These bags are waterproof and have a valve which stops the urine in the bag going back into the stoma. They are also odour-proof. They are fixed to the body with adhesive around the stoma. The bags have a tap or valve which lets you empty the urine into the toilet when the bag is full whilst leaving the bag in place.